PrEP, or pre-exposure prophylaxis, is transforming HIV prevention strategies in 2025. With new delivery methods, increased accessibility, and greater public awareness, PrEP is now one of the most effective tools in reducing new HIV infections. But what exactly is PrEP, and how is it being used to change the face of HIV prevention today?
Table of Contents
- Understanding PrEP: The Basics
- Current PrEP Options and Innovations
- Who Should Consider PrEP in 2025?
- Addressing Barriers and Expanding Access
- Conclusion
- FAQs
Understanding PrEP: The Basics
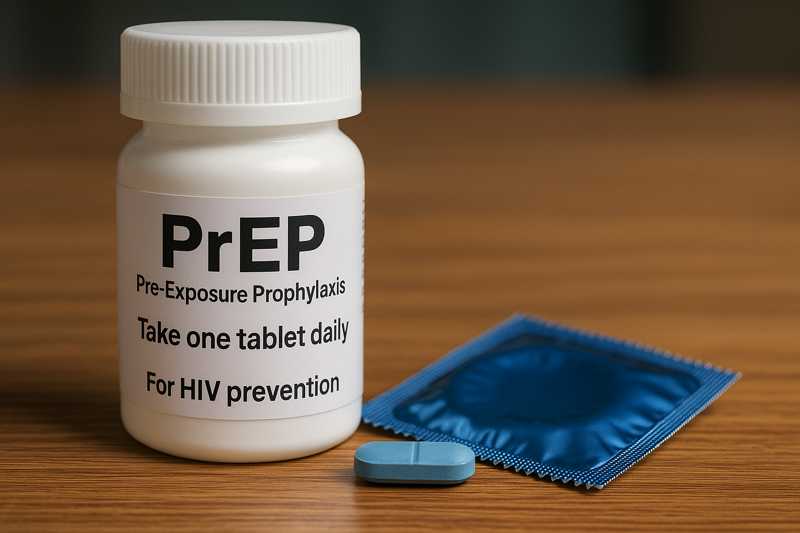
Pre-exposure prophylaxis, or PrEP, involves taking medication before potential exposure to HIV to prevent infection. It works by establishing protective levels of antiretroviral drugs in the body, making it highly effective at blocking the virus from taking hold. The concept is simple but powerful: stop HIV before it has a chance to start.
PrEP first gained FDA approval in 2012 with the drug Truvada (tenofovir disoproxil fumarate/emtricitabine). In 2025, PrEP options have evolved to include newer, better-tolerated medications and even long-acting injectables. When taken as prescribed, PrEP reduces the risk of HIV transmission through sex by over 99%, and by at least 74% for people who inject drugs.
These results make PrEP an essential part of comprehensive HIV prevention strategies, particularly for communities at higher risk. Importantly, it also provides peace of mind and a sense of empowerment for those using it.
Current PrEP Options and Innovations
PrEP in 2025 is no longer a one-size-fits-all approach. Multiple options exist to fit different lifestyles and health needs. Traditional daily oral pills remain effective, but newer alternatives are providing more flexibility.
Daily Oral PrEP: The standard daily pill is still widely used and includes Truvada and Descovy (tenofovir alafenamide/emtricitabine). These are prescribed based on factors like age, sex at birth, and kidney function. They are easy to take, require routine testing, and are widely covered by insurance.
On-Demand PrEP: Known as 2-1-1 dosing, this regimen is for men who have sex with men and involves taking pills before and after sexual activity. Although not FDA-approved in the U.S., it is gaining global traction and may suit those with less frequent exposure.
Injectable PrEP: Apretude (cabotegravir) is a long-acting injectable PrEP that was approved for use in 2021 and has gained popularity in recent years. It requires a shot every two months, offering a discreet and convenient alternative to daily pills.
New delivery methods are also on the horizon. Research into PrEP implants and monthly pills continues, with the goal of making HIV prevention even more accessible and user-friendly. For more updates on prevention innovation, visit the AIDS.org blog.
Who Should Consider PrEP in 2025?
PrEP is recommended for anyone at high risk of HIV exposure. However, who qualifies as high risk can vary depending on behaviors, partners, and geographic location. The CDC and WHO provide updated guidelines to help identify ideal candidates.
Groups that benefit most from PrEP include:
- Individuals with an HIV-positive sexual partner
- People who have multiple sexual partners or engage in condomless sex
- Sex workers and people who trade sex for money or goods
- People who inject drugs and share needles
- Individuals diagnosed with STIs in the past six months
- Men who have sex with men (MSM), especially in urban areas with high HIV prevalence
Additionally, PrEP may be suitable for adolescents and young adults who meet these criteria. Pediatric formulations and youth-centered services are being developed to expand reach to vulnerable populations.
Education plays a key role in awareness. Many people still don’t know PrEP exists or misunderstand its purpose. Healthcare providers and public health campaigns are working to close that gap, ensuring more people understand their prevention options.
Addressing Barriers and Expanding Access
Despite its effectiveness, PrEP remains underutilized. Barriers include cost, stigma, lack of access to healthcare providers, and misconceptions about who PrEP is for. In 2025, several initiatives are tackling these challenges head-on.
Insurance and assistance programs have helped make PrEP more affordable. Federal and state-level policies ensure Medicaid coverage, and many private insurers cover both oral and injectable forms. Meanwhile, community health centers and LGBTQ+ clinics offer low-cost or free services.
To combat stigma, organizations are reframing PrEP as proactive and responsible. Instead of being seen as a drug for the promiscuous, it’s now positioned as part of a broader health and wellness routine. Telehealth options also provide discreet access for those uncomfortable discussing sexual health in person.
Furthermore, campaigns targeting Black, Latino, and Indigenous communities are helping bridge gaps in access and outcomes. These groups often face higher rates of HIV yet remain less likely to be on PrEP. Inclusive messaging, community partnerships, and culturally competent care are key to reversing these trends.
Policy changes have also helped. In some states, pharmacists can now prescribe PrEP without a doctor’s visit, making it easier than ever to start treatment. Continued investment in public health infrastructure will be critical to maintaining these gains.
For more information about our mission and support services, visit AIDS.org.
Conclusion
PrEP has emerged as a cornerstone of HIV prevention in 2025. With daily pills, injectables, and new delivery methods on the way, individuals have more choices than ever to stay HIV-free. The science is clear: PrEP works. But success also depends on awareness, access, and empowerment.
Public health leaders, providers, and communities must continue working together to eliminate stigma, expand services, and educate the public. When implemented effectively, PrEP can bring us closer to ending the HIV epidemic.
FAQs
What does PrEP stand for?
PrEP stands for Pre-Exposure Prophylaxis. It involves taking medication before potential exposure to HIV to prevent infection.
How effective is PrEP at preventing HIV?
When taken consistently, PrEP reduces the risk of acquiring HIV through sex by over 99% and by 74% for injection drug users.
Are there side effects of taking PrEP?
Most people tolerate PrEP well. Some may experience mild side effects like nausea or fatigue, but these often go away after a few weeks.
Can I stop using condoms if I’m on PrEP?
While PrEP protects against HIV, it does not protect against other STIs. Using condoms is still recommended for full protection.
Where can I get PrEP?
PrEP is available through healthcare providers, sexual health clinics, and in some states, directly from pharmacists. Visit Healthcare.pro for help finding services near you.
Disclaimer
“This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.”



