When HIV first emerged in the early 1980s, the outlook was bleak. Yet, over the past four decades, HIV treatment methods have evolved dramatically—from a single, often-toxic drug to a sophisticated array of therapies that can suppress the virus indefinitely. Today, people living with HIV can lead long, healthy lives. But how did we get here?
Understanding the history of HIV treatment methods isn’t just about looking back. It’s about appreciating the progress, honoring the scientific breakthroughs, and recognizing the lives changed along the way. In this article, we’ll explore the pivotal moments in HIV therapy, from the earliest days of the epidemic to the promising future of injectable treatments and potential cures.
Table of Contents
- The Beginnings: Early HIV Treatments and Challenges
- The Antiretroviral Therapy Revolution
- Modern Advancements in HIV Treatment Methods
- Looking Ahead: Long-Acting Therapies and Beyond
- Conclusion
- FAQs
The Beginnings: Early HIV Treatments and Challenges
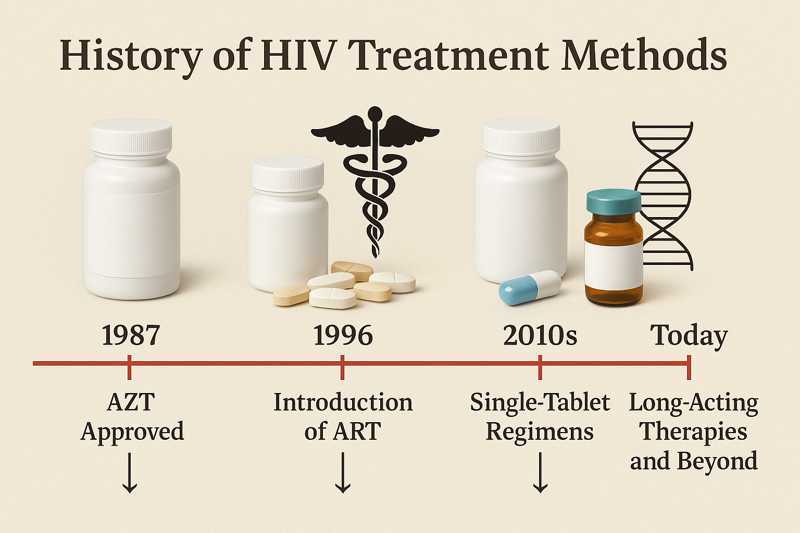
In the early 1980s, HIV was a mysterious and deadly virus. With no known cure or effective treatment, the medical community was left scrambling. The first major breakthrough came in 1987 with the FDA approval of zidovudine, commonly known as AZT.
AZT marked a critical milestone. It was the first antiretroviral drug and provided hope, but it also had significant limitations. High doses were needed, which led to severe side effects like anemia and nausea. Additionally, AZT monotherapy could only delay disease progression, not stop it.
By the early 1990s, it became clear that single-drug therapy wasn’t enough. Resistance developed quickly, and treatment success was short-lived. At the time, patients were often prescribed multiple pills per day with complicated regimens. Adherence was difficult, and outcomes remained inconsistent.
Despite these challenges, this era laid the foundation for modern HIV treatment methods. Researchers began to understand how the virus replicated, and pharmaceutical companies started developing drugs that could attack HIV at different stages of its life cycle.
The Antiretroviral Therapy Revolution
The mid-1990s marked a turning point. In 1996, the introduction of Highly Active Antiretroviral Therapy (HAART) changed everything. HAART combined three or more drugs from different classes, effectively halting HIV replication. For the first time, patients had a real chance at long-term survival.
HAART regimens were initially complex and came with a hefty pill burden. However, their impact was undeniable. Hospitalization rates declined, and the number of AIDS-related deaths dropped dramatically. This shift turned HIV from a death sentence into a manageable chronic condition.
Over the years, treatment options continued to improve. Fixed-dose combinations reduced pill counts, making adherence easier. The launch of Truvada (emtricitabine and tenofovir disoproxil fumarate) not only supported treatment but also played a major role in prevention through Pre-Exposure Prophylaxis (PrEP).
By the 2010s, single-tablet regimens became standard. Drugs like Biktarvy and Genvoya made it possible to maintain viral suppression with just one pill a day. These regimens combined efficacy with convenience and minimized side effects, making them highly desirable for long-term use.
To explore other impactful developments, visit AIDS.org blog, which covers historical and emerging HIV care topics.
Modern Advancements in HIV Treatment Methods
In recent years, the focus has shifted toward simplifying treatment even further. Long-acting injectables, such as Cabenuva (cabotegravir and rilpivirine), offer an alternative to daily pills. These monthly or bi-monthly shots maintain viral suppression and improve quality of life, especially for those struggling with pill fatigue.
Additionally, integrase inhibitors like dolutegravir have become central to first-line therapy. These drugs offer high potency, a strong resistance profile, and fewer side effects. Combined with nucleoside reverse transcriptase inhibitors (NRTIs), they form the backbone of many current HIV treatment methods.
Moreover, the development of personalized medicine is making strides. Pharmacogenomic testing helps clinicians choose the best regimen based on a patient’s genetics, lifestyle, and comorbidities. This tailored approach minimizes side effects and improves long-term adherence.
Digital tools and support platforms also enhance patient engagement. Apps can remind users to take medications, track lab results, and communicate securely with care teams. For guidance on care options and trusted advice, patients can visit Healthcare.pro.
On the global front, the availability of generic drugs has improved access in low-resource settings. The World Health Organization continues to endorse simplified regimens that are both effective and affordable, contributing to the broader fight against HIV/AIDS.
Looking Ahead: Long-Acting Therapies and Beyond
The future of HIV treatment is promising. Scientists are developing even longer-acting therapies, including injectable treatments that could last up to six months. Implants, similar to those used for birth control, are also in early testing phases.
Beyond suppression, researchers are exploring functional cures. Trials involving therapeutic vaccines, broadly neutralizing antibodies, and gene-editing tools like CRISPR aim to eliminate the virus or control it without medication. Although these treatments are experimental, they represent the next frontier in HIV medicine.
Equally important is addressing stigma and healthcare equity. Ensuring that new therapies reach marginalized communities remains a priority. Cultural competency, patient education, and community-based care models will play a pivotal role in ensuring everyone benefits from these innovations.
For more on how AIDS.org supports patient advocacy and educational outreach, visit our mission page.
Conclusion
The history of HIV treatment methods reveals a remarkable journey of resilience, innovation, and hope. From toxic monotherapies to streamlined, effective regimens—and now to long-acting injectables and potential cures—the landscape has transformed dramatically. With continued research, equitable access, and patient-centered care, the future holds even more promise for people living with HIV.
FAQs
What was the first HIV treatment approved by the FDA?
AZT (zidovudine) was the first approved HIV treatment, introduced in 1987.
What does HAART stand for in HIV treatment?
HAART stands for Highly Active Antiretroviral Therapy, a regimen combining multiple drugs to control HIV.
Are there once-a-month HIV treatments available today?
Yes, Cabenuva is a long-acting injectable given monthly or every two months, depending on the regimen.
Can HIV be cured with current treatments?
Current HIV treatments can suppress the virus effectively but are not a cure. Research on potential cures is ongoing.
Where can I find trusted information about HIV treatment options?
For reliable resources and updates, visit AIDS.org and consult healthcare professionals through Healthcare.pro.
Disclaimer:
“This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.”



